Understanding the Long-Term Effects of COVID-19
For some, the coronavirus causes far more severe damage to the rest of the body than just the lungs
Lesser-known aftereffects of the coronavirus include inflammation and damage within the brain.
February 6, 2021
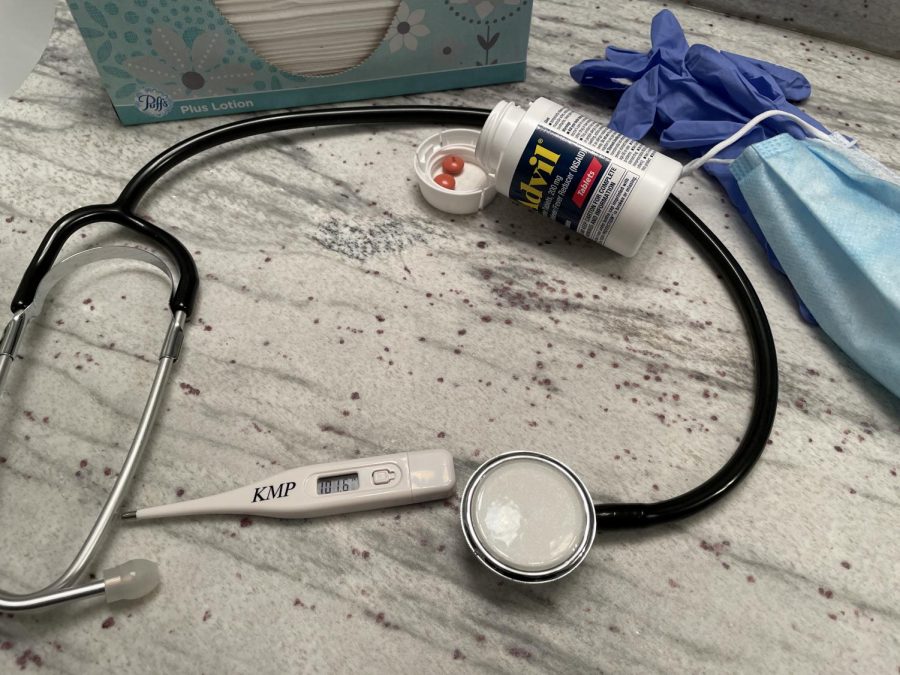
Contracting the coronavirus, whether mild or severe, can be a difficult battle. Days and nights of chills, fevers and body aches can take a toll on an individual both mentally and physically. Then, when it may seem as though one has overcome the virus, there are a number of long-term effects that can affect the body, including the brain.
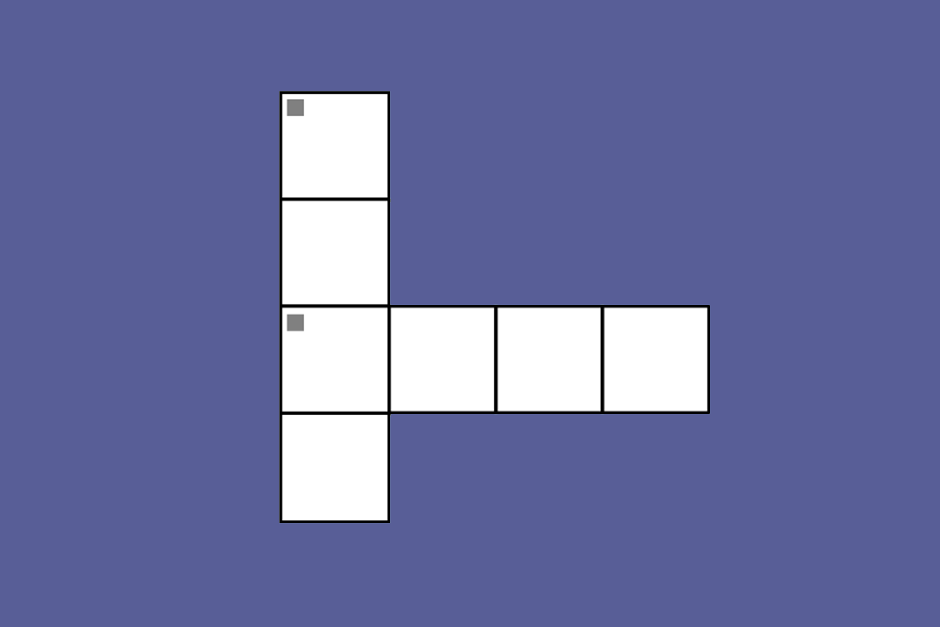
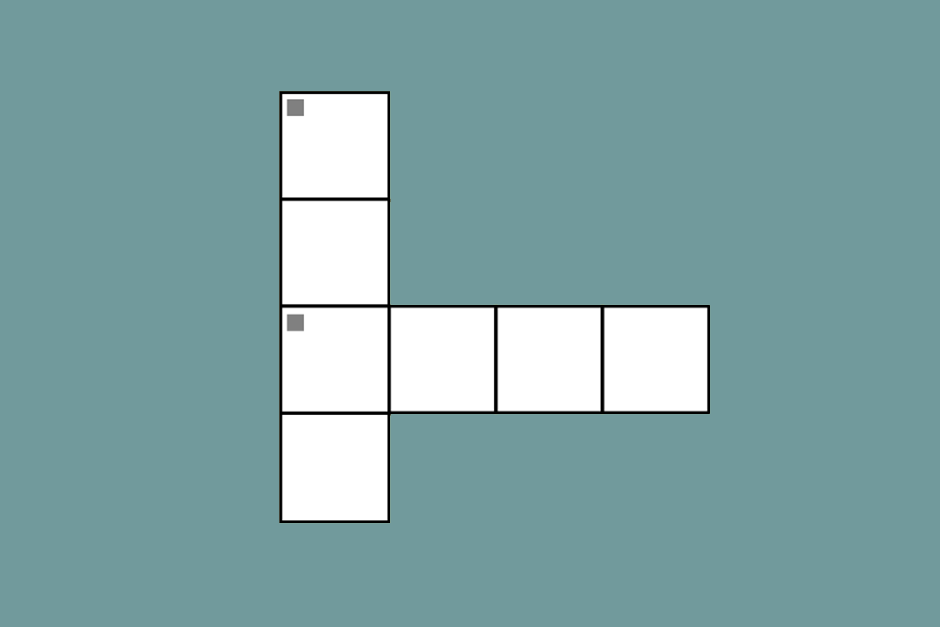
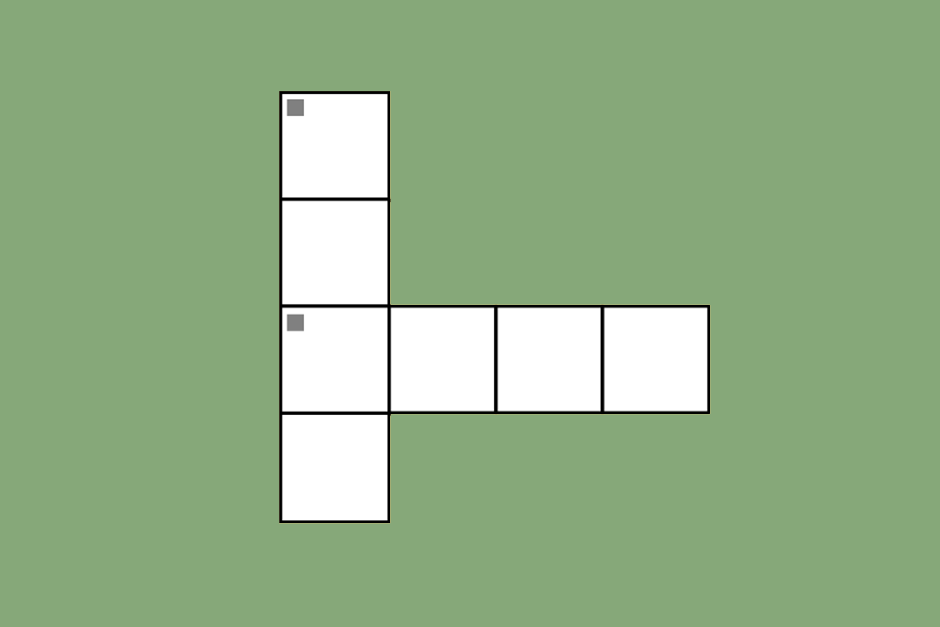
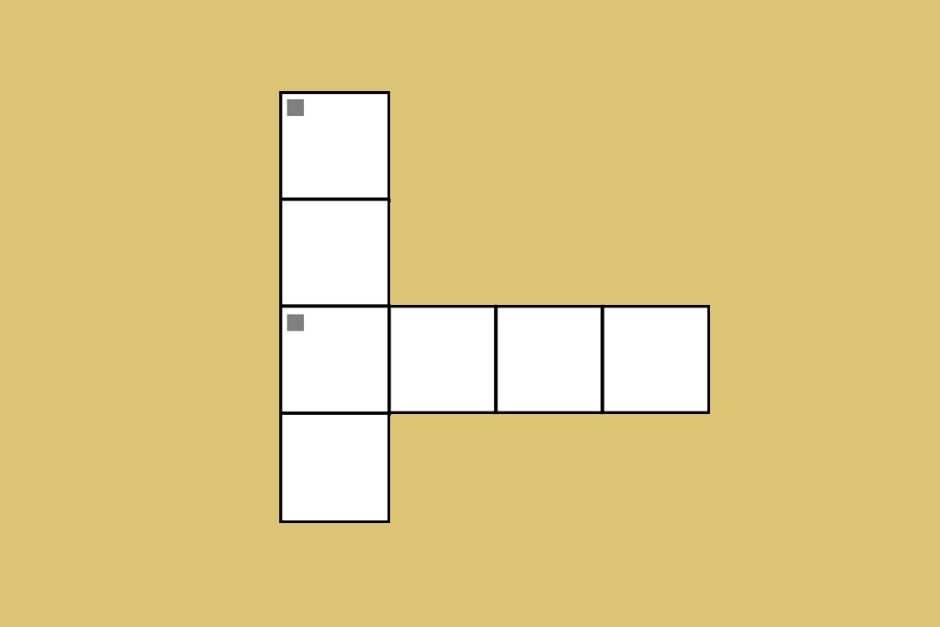
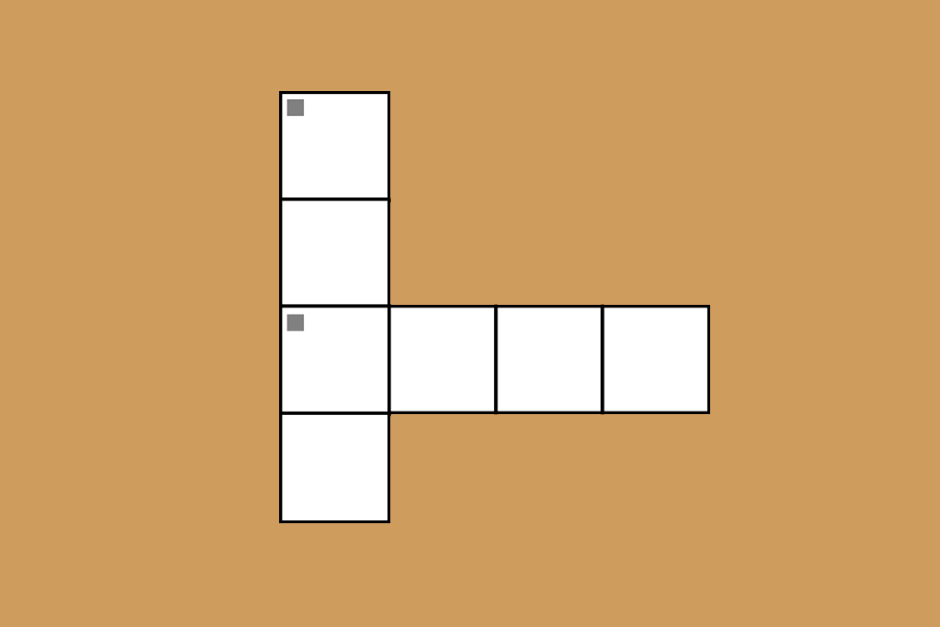
Pathway of the Virus
A virus enters the body by infecting healthy cells. The coronavirus invades by latching its spiky surface proteins to the cell receptors and multiplying, especially in the lungs.
These viral proteins make their way into the whole body through ACE-2 receptors in order to hijack and destroy healthy cells. As the virus moves down the respiratory tract, it can progress beyond common cold symptoms and lead to infections in the alveoli of the lungs, causing pneumonia.
The aftereffects of inflammation in the olfactory nerve and the central nervous system (CNS) cause severe encephalitis, vascular damage and destruction of the blood-brain barrier.
However, problems caused by COVID-19 extend far beyond the lungs. “At the beginning, everything was acute, and now we’re recognizing that there may be more problems,” said Helen Su, an immunologist at the National Institute of Allergy and Infectious Diseases in Maryland, in an interview for Nature.
The aftereffects of inflammation in the olfactory nerve and the central nervous system (CNS) cause severe encephalitis, vascular damage and destruction of the blood-brain barrier. The olfactory nerve is one of the 12 cranial nerves and passes from the nasal mucosa to the forebrain. Similarly, encephalitis refers to inflammation of the brain which can cause symptoms like fevers, headache and epileptic seizures.
Permeating Into the Brain
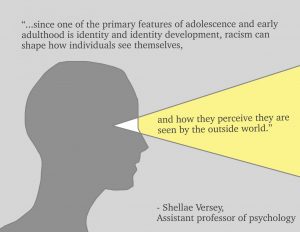
The neurological symptoms of the virus revealed that it has tropisms, which means that the viral strain of coronavirus has the ability to infect different types of cells and tissues. According to the Elsevier Public Health Collection, the SARS-CoV-2 genome receptor was located in the brain tissue of infected patients. COVID-19 has the power to enter neural tissue, causing inflammatory lesions in the brain affecting the thalamus and hippocampus. The implications of this invasion are harmful because the thalamus relays sensory and motor signals to the body and helps individuals stay conscious and alert. Some symptoms include difficulty maintaining balance, loss of memory and changes in speech.
The blood-brain barrier is one of the brain’s most important anatomical features, as it protects against any circulating toxins or pathogens that could cause brain infections while allowing vital nutrients to reach the brain.
Inflammation of the brain caused by the coronavirus is predominantly a white-matter disease that results in the demyelination of neurons. A demyelinating disease is one that damages the myelin sheath which acts as a protective covering for nerve fibers, optic nerves and the spinal cord. When this protective layering is damaged, an individual can have slow nerve impulses leading to neurological problems like vision loss, multiple sclerosis and diminished control over one’s bladder.
The virus can also spread to the brain by interacting with the ACE-2 protein in the smooth muscle lining of the vascular system. The activated immune response to this at the protein receptor causes the loss of blood-brain barrier integrity. The blood-brain barrier is one of the brain’s most important anatomical features, as it protects against any circulating toxins or pathogens that could cause brain infections while allowing vital nutrients to reach the brain. Degradation of this feature makes the border of the brain extremely vulnerable to additional viruses and pathogens.
Hear about the coronavirus vaccine and its aftereffects on Retrospect:
https://open.spotify.com/episode/2ytNB5I7y9UMRRoolMpEjt?si=mP1np8e_Q9CgiLwsDR-wHg
Progress Toward Prevention
A recent study done by the American Academy of Neurology collected cerebrospinal fluid from eight COVID-19 patients to test for coronavirus antibodies. Cerebrospinal fluid is a clear substance that surrounds the brain and spinal cord. Its function is to serve as a cushion to prevent injury and remove waste from the brain. The spinal fluid was tested for autoimmune encephalitis antibodies and several markers of ongoing neurodegeneration.
A high antibody count of SARS-CoV-2 was determined to be directly proportional to the amount of damage done to the blood-brain barrier.
As global COVID-19 deaths surpass 2 million, scientists and doctors are carrying out more observational studies to determine the role of the pathogenic antibodies of the virus. This will help the medical community to identify and plan early therapeutic and pharmacological drug therapies to prevent life-threatening residual effects of the virus.