Debunking Your Body Mass Index
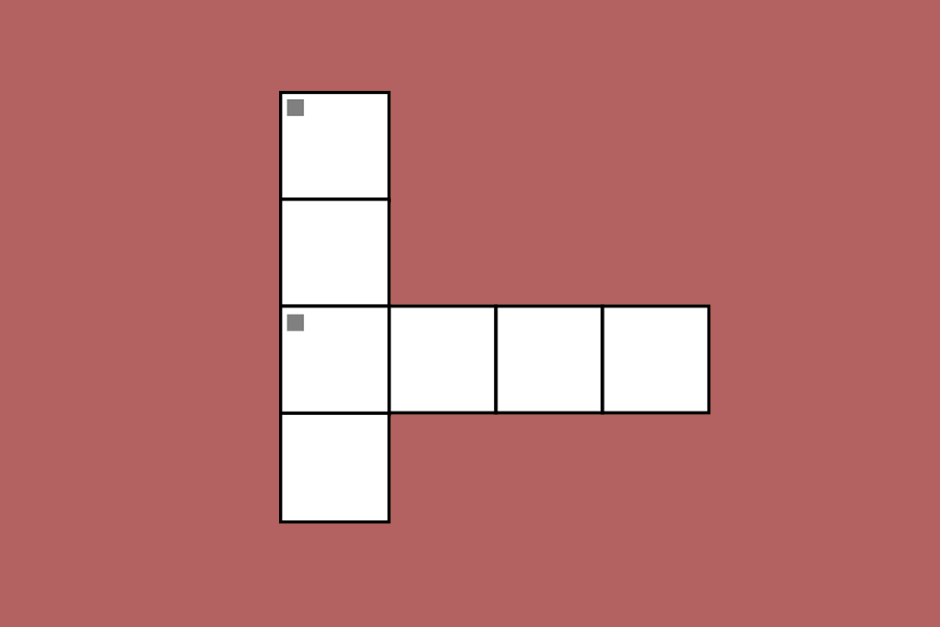
BMI is a person’s weight divided by the square of their height.
March 15, 2018
You may have heard of body mass index (BMI) in “Get fit quick” advertisements, obesity public service announcements or from your physician. BMI seems like a foolproof and scientific approach to measuring one’s body makeup and overall health. The measurements BMI assigns are clean and simple, ranging from 12 (severely underweight) to 42 (severely obese). BMI also provides you with succinct categories: “underweight, healthy, overweight, and obese.” Organized on a graph of weight versus height, BMI lends itself as an answer to a nuanced health phenomenon. However, BMI aims to oversimplify this label; health is a complex label that comes with many varying indicators and assertions.
BMI has an odd origin. In 1835, Lambert Adolphe Jacques Quetelet, a Flemish astronomer and statistician, created BMI. Quetelet created BMI in order to place citizens into specific categories according to their physical features. In theory, BMI was designed to streamline the pathway to bring about health policy. Quetelet intended to quantify various other physical attributes about the “average man” in order to achieve similar goals. He named this statistical approach “social physics.”
Later in the 1970s, statisticians adopted BMI as the standard measure of obesity in population-based studies. At the time, BMI provided researchers with a quick and moderately accurate way of assessing obesity rates in a population. By the 1990s, the World Health Organization (WHO) had adopted BMI as the standard for obesity analysis. High profile agencies, like the WHO and the Centers for Disease Control (CDC), gave BMI the legitimacy it boasts to this day.
Mathematically, BMI is an individual’s weight in kilograms divided by the square of their height in meters. The key issue with BMI is that it does not account for lean body mass, which includes muscle, organs and bones. Therefore, an individual can have a high BMI with very little fat at all. This person would also fall outside of the “healthy” threshold and in the “overweight” or “obese” categories. Mislabeling individuals as “overweight” or “obese” comes with serious statistical, political and psychological ramifications.
To make matters worse, BMI is commonly used to assess the mortality risk for large populations. BMI is merely based upon height and weight; it does not account for very important cofactors like family history of diabetes, heart problems, or cancer. There is evidence to suggest that genetics accounts for 50 percent of one’s susceptibility for coronary heart disease. In addition, a high percentage of muscle mass is inversely proportional to diabetes. BMI, which labels individuals with high muscle mass as “overweight,” is an inaccurate metric for mortality risk for large groups of people; new sources of data are very much needed.
On the Center for Disease Control (CDC) website, BMI conspicuously stands out on the “Healthy Weight” information page. By clicking on “Assessing Your Weight,” the CDC provides one with relevant information about the measurement, a BMI calculator and guidelines to interpret the BMI score. Regrettably, the CDC misleads individuals by attesting, “BMI appears to be as strongly correlated with various metabolic and disease outcome[s] as more direct measures of body fatness.” Though the CDC is using careful language to describe BMI’s effectiveness, it still lists BMI as one of the major metrics one can use to measure his or her body composition.
Nonetheless, the CDC mentions alternative methods for assessing body fat mass. These alternatives include skinfold thickness measurements, underwater weighing and dual energy x-ray absorptiometry (DXA). The Canadian Medical Association attests that DXA provides more precise data on body composition: it measures bone mineral content, bone mineral density, lean tissue mass and fat tissue mass. Increasingly, medical professionals favor DXA over BMI for assessing body composition, for DXA is more accurate and gives more information about the individual than BMI.
With access to newer, more precise measurements of body composition obesity, researchers have no reason to use BMI as the standard. At best, BMI can only give an estimation of body composition. Luckily, the medical community is increasingly skeptical of BMI’s ability to diagnose overall health. New technologies like DXA will provide physicians and researchers with more accurate estimates. As medicine moves forward and new, more accurate metrics develop, BMI becomes increasingly outdated and inaccurate. Medicine operates upon accuracy, so BMI should be left in the past.